
Executive Summary
Healthcare is a stressful industry, leading to higher rates of anxiety, depression and stress than many other professions. The goal of this project was to offer a clinically-effective and cost-effective online cognitive behavioral therapy for anxiety, stress and depression to at least 1,000 St. Luke’s University Health Network (SLUHN) employees and/or spouses by Sept. 15, 2018. The use of technology improved access to mental health services, allowed users convenience and instant access to care and made seeking care more comfortable for users who may not otherwise have sought mental health treatment. SilverCloud proved to be effective, cost efficient and scored high marks on user satisfaction. The success of the SilverCloud implementation at SLUHN is demonstrated by the utilization and outcomes data that were collected. Plans for adding additional SilverCloud programs and expanding SilverCloud availability to additional populations are under way.
Define the Clinical Problem and Pre-Implementation Performance
St. Luke’s University Health Network (SLUHN) is a non-profit health system with more than 16,000 employees providing care and services at 12 hospitals and more than 300 outpatient locations. In addition, SLUHN has a self-insured medical plan. Historically, healthcare professionals have higher rates of work-related stress, anxiety and depression than the general population. Internal baseline data confirmed that emotional and behavioral health issues were affecting employees and their dependents, presenting an opportunity for improvement.
The SLUHN Amerihealth Chronic Illness Report for FY16 reported that Mental Health was the #1 chronic condition amongst SLUHN covered lives. Mental Health support was provided to 2,296 SLUHN plan members that year at a cost of $2,243,488.
In 2016, more than 55% of Caring Starts with You (SLUHN’s Employee Wellness/Population Health program) participants reported feeling anxious and stressed sometimes or often. In 2016, mental health conditions were among the top 10 medical conditions on the health plan and anti-depressants were among the top 10 prescribed medications. Mental health conditions were affecting more SLUHN employees than high blood pressure or diabetes.
This baseline data indicated that there was a need for additional mental health services in our employee population. However, there were many barriers affecting the delivery of mental healthcare, including cost, stigma, provider supply-demand mismatch, scheduling delays and the lack of ability to reach the appropriate patients. The effectiveness of cognitive behavioral therapy is well established for many mental illnesses, including mood and anxiety disorders.
Traditional services often require that a patient be seen in person. Face-to-face appointments must be scheduled, potentially causing delayed treatment, an increase in costs and a bottleneck in the system. Due to an increasing need, recognition of the effectiveness of mental healthcare and staffing shortages both locally and nationally, the limited mental healthcare providers available are being overwhelmed by the growing demand for services. Furthermore, the standard process of establishing the traditional face-to-face encounter is both labor and cost intensive, regardless of acuity, demographic or payer.
The problem the network faced was that there was inadequate access to mental healthcare.
To address the shortage of trained mental health professionals and the other barriers impacting mental healthcare, St. Luke’s began exploring innovative solutions. The network leveraged support from senior leadership and stakeholders from human resources, behavioral health, employee wellness, information technology and the innovations team to provide input and expertise into the project. The goal was to increase access to mental healthcare services by offering clinically effective and cost effective online cognitive behavioral therapy for anxiety, stress and depression to SLUHN employees and spouses.
The project aimed to increase access to clinically effective and cost effective online cognitive behavioral therapy for anxiety, stress and depression to at least 1,000 SLUHN employees and spouses by Sept. 15, 2018.
Generalized anxiety disorder (GAD) is a very common mental health disorder. The GAD-7 is a seven-question self-assessment tool accepted as an industry standard for measuring the severity of anxiety in clinical and research settings (Spitzer, et al.). Depression is one of the most prevalent mental health disorders commonly encountered. The PHQ-9 is the nine-item depression module of the patient health questionnaire. It’s validity and ease of use has made it the industry standard for assessing depression severity (Kroenke, et al.).
The plan was to use supportive technology to overcome barriers to accessing mental healthcare. If utilization targets were achieved, the network could assess clinical effectiveness and cost effectiveness compared to face-to-face treatment using industry standard measures such as the GAD-7 and PHQ-9. These assessments are the same tools used in the quality metric defined as patients exhibiting signs of depression via PHQ-9 screenings. The HEDIS measure related to this project is Depression Screening and Follow-up for Adolescents and Adults Adapted from a provider-level measure developed by Quality Insights of Pennsylvania (QIP) (NQF #0418, CMS2), first implemented in HEDIS® 2018. Please note that because this project was implemented to anonymous members of the employee population, these measures were administered and tracked via the SilverCloud platform, not via or interfaced with the electronic medical record.
Design and Implementation Model Practices and Governance
A committee consisting of subject matter experts (SME) in behavioral health, social work, public health and health education conducted a literature review that indicated that internet-delivered cognitive behavioral therapy is a viable and effective alternative to face-to-face treatment. Furthermore, internet-delivered cognitive behavioral therapy with some input from a therapist can be as clinically effective as face-to-face cognitive behavioral therapy and more cost-effective.
A SLUHN team consisting of the above SMEs, the chair of community health and preventive medicine, IT analysts and the innovations team engaged with AVIA in February 2016 in a new cohort they formed focusing on mental health. Two St. Luke’s behavioral health staff attended the AVIA conference in May 2016 in Chicago to vet various programs. Over a period of eight months, 12 different options were considered. Programs were evaluated based on provider workflow, patient engagement, data and analytics, solution scalability, technical infrastructure and proven success.
SLUHN selected SilverCloud, an industry-leading, evidence-based solution. SilverCloud is an online platform that offers 24/7 access to clinically proven programs based on cognitive behavioral therapy, mindfulness, and positive psychology. It includes both self-guided and coached interventions. A SLUHN-sponsored supporter would interact with a large group of employees through their treatment and education, matching the intensity of the intervention with individual needs. The supporter guides patients through asynchronous communication via the SilverCloud application and provides non-clinical feedback, recommendations and support.
This case study is unique because the patient population consisted of SLUHN employees and their spouses. Those interested in using SilverCloud could self-refer (either based on existing diagnosis or as an access point to care they may not otherwise have received). Account creation is anonymous, using a unique SLUHN login page and PIN. The program content is contained in modules within the SilverCloud platform. Users agree to a contract of understanding when they create their account, which details what is expected of them and what they can expect of the program and the supporter. The MSW supporter is employed by the network to assist users along the way. Participant progress is measured at intake and periodically throughout their program using industry standard tools such as the GAD-7 and PHQ-9. Participants are evaluated for caseness, recovery, showing reliable change and reliable recovery. The supporter also monitors acuity/fit of the participants for the program. Participants in need of services exceeding SilverCloud’s capability would be referred to the Employee Assistance Program or other resources as appropriate. Thresholds were set within the SilverCloud system to notify the supporter of a high risk sign up and/or assessment result. SLUHN aligned processes and outcomes metrics with SLUHN’s Behavioral Health Department’s processes and metrics. SilverCloud’s ability to offer this customization addressed SLUHN’s needs, making SilverCloud the choice for this technology-based mental health pilot.
The goals were to use SilverCloud to:
- Reduce healthcare utilization costs and stigma
- Compare cost effectiveness of treatment compared to face-to-face treatment
- Create a viable alternative to face-to-face treatment to free up the back log and increase accessibility
Clinical Transformation enabled through Information and Technology
After a custom build, SilverCloud was launched in 2017. Programs for anxiety, stress and depression were available for free, anonymously and confidentially, to SLUHN employees and spouses. After creating their account, participants access and progress through the program modules at their own pace, at their convenience, from a computer, tablet or smart phone. Participant satisfaction, clinical outcomes and cost effectiveness would be measured and evaluated. Additionally, account creation/number of participants was a primary area of focus. To evaluate clinical outcomes, user satisfaction and cost effectiveness, we first needed users.
These KPIs were set:
- Number of participant activated (sign-up)
Project goal: 800 | target: 1,000 | stretch: 1,200
- Average reduction outcomes
Goal: 4 points | target: 5 points | stretch: 6 points
- % participants completed program and reduced PHQ9 & GAD7 scores by 4-6 points
Goal: 40% | target: 45% | stretch: 50%
- User satisfaction
Measure end of module scores
- Cost effectiveness of treatment compared to face-to-face treatment
A multi-tiered marketing plan was developed to promote and normalize SilverCloud as a resource for mental healthcare. SLUHN sought to not only create awareness about SilverCloud and educate people about the benefits of using it, but to begin a crucial conversation about self-care and addressing mental health needs. Safe, friendly approaches were incorporated into the marketing plan to reduce stigma and drive employees and their spouses to use the platform. Initial marketing strategies included an in-home mailer, refrigerator magnet, quarterly emails, intranet postings, presentations at new hire orientation, posting SilverCloud materials throughout the network in staff-only areas and providing SilverCloud information during Benefits Fairs. This led to an initial group of early adopters who created accounts and began using the platform, while also contributing to ongoing account creation and platform use by the general employee population. Subsequent marketing efforts included targeted approaches to ensure that the resource was being brought to the attention of those who might benefit the most from it.
Additionally, to keep SilverCloud top of mind, the program was included in presentations to high impact groups, including management meetings, nursing residency groups and medical residents. Though the anonymity and confidentiality of the SilverCloud platform were always emphasized in marketing efforts, the planning team recognized that there may have been potential users who would appreciate having the opportunity to interact, put a face to the program and ask questions of the supporter and the creators of the SilverCloud platform. A series of on-site demonstration booths were scheduled across the network, which were called “SilverCloud Roadshows.” They were in prominent locations including cafeterias, lobbies and conference rooms. Finally, SLUHN leadership allowed completion of a SilverCloud program to count as a Healthy Living Activity in SLUHN’s 2018 annual Employee Wellness Health Assessment.
SilverCloud demonstrated several impressive outcomes based on SLUHN KPIs.
Participation: The SLUHN SilverCloud project goal for participation was 1,000 accounts, with a stretch goal of 1,200. 1,161 accounts were created in year one, and 1,300 additional accounts were created in the first three months of year two. More than 3,000 employees and spouses have used the program, which is a significant number of users on which to measure clinical outcomes. The online technology solution offered users the convenience of anytime access from anywhere. The SLUHN implementation of SilverCloud did not require that users identify themselves at account creation, thereby enabling a level of comfort from users who may not otherwise have accessed SilverCloud or face-to-face mental health services. The SLUHN implementation also included the hiring of a Social Worker (MSW) to interact asynchronously with participants through the technology/platform. This appealed to those seeking guidance, accountability and/or cognitive behavioral therapy that wasn’t only self-service.
Participant Satisfaction: SLUHN SilverCloud users reported a 97% satisfaction rate with the SilverCloud program. At the completion of each module, the SilverCloud platform assesses user satisfaction with various aspects of the program and user experience. Most users “agree” or “strongly agree” that their program was interesting, relevant, helpful and contributed to progress toward their goals.
Clinical Outcomes: Industry standard measurements for depression (PHQ9) and anxiety (GAD7) are used at baseline and regularly during program progression. The following definitions are established for measuring clinical effectiveness:
- Case – occurs if a participant scores above the clinical threshold on the depression and/or anxiety assessment at signup
- Recovery – occurs if the participant subsequently scores below the clinical threshold on the depression and/or anxiety assessment
- Reliable change – occurs if a participant’s score drops a predetermined number of points on the depression and/or anxiety assessment
- Reliably recovered – occurs if the predetermined point reduction drops the individual below the clinical threshold on the depression and/or anxiety assessment
In both the Space from Depression and Space from Anxiety programs, there was a downgrading of clinical acuity based on PHQ-9 and GAD-7 scores taken before, during and after program use. In reviewing improvement and clinically significant improvement by baseline severity in the Space from Depression Program, out of 1,042 responders to PHQ9, 71% of moderately severe users report clinically significant improvement, and 50% of severe users report clinically significant improvement. In reviewing improvement and clinically significant improvement by baseline severity in the Space from Anxiety Program, out of 1,038 responders to GAD-7, 52% of moderate users report clinically significant improvement, and 62% of severe users report clinically significant improvement. We also noted a leveling of Employee Assistance Program (EAP) utilization concurrent with the rollout of SilverCloud.
Cost Effectiveness: SLUHN used network data to show the cost of face-to-face mental health treatment per employee. Cost effectiveness was demonstrated by comparing the SilverCloud cost for the users meeting the clinical threshold for diagnoses at SilverCloud sign up to the cost that would have been incurred had they sought face-to face treatment. Cost effectiveness was also demonstrated by comparing what the users who had reliable recovery (defined as reliable reduction—4 points for PHQ-9 or 6 points for GAD-7—and fell below the clinical threshold) would have cost the network had they gone for face-to-face treatment, compared to the cost for them to use SilverCloud. Cost effectiveness was also demonstrated by showing that the network’s all-time investment for the SilverCloud program and FTE for the 2-year pilot is less than what it would have cost to treat the reliably recovered users in face-to-face treatment. SLUHN saved $17 for every $1 spent on SilverCloud for users who met the clinical threshold for diagnosis.
The success of this project is attributable to thorough assessment, planning, implementation, process and outcome evaluation. The team was careful to know the population, stay in tune with the barriers, systematically address barriers and weave the solution through the organization in various ways. We were able to gain acceptance for the technology by making it palatable to different parts of the SLUHN population. We began an important conversation about mental health and self-care, normalizing them and making them acceptable. We intended to make the program sustainable, not treat it as a gimmick or flavor of the month, but an ongoing commitment for the organization and our employees. Underscoring this, the platform and project were included recently as a case study in the SLUHN HIMSS Stage 7 EMRAM Network reaccreditation process.
Improving Adherence to the Standard of Care
Part of providing quality care is to deliver services at the appropriate level of cost and care. Treating individuals at the level their needs require is simply efficient and saves the health system from unnecessary waste in terms of time, labor and resources.
Initially, SLUHN targeted increased access to behavioral health services as a goal for the SilverCloud project, with a baseline of 800 plan participants/covered employees utilizing the service.
During the pilot, 1,161 covered employees utilized the service, exceeding SLUHN’s initial target goal. To date, more than 2,900 SLUHN covered employees have used SilverCloud.
Though participants would be anonymous, we hoped to see SilverCloud organically grow into a resource able to attract and ultimately direct participants to services of an appropriate level of care for their specific needs.
Two examples of targeted populations are users who might otherwise never seek care and those who might be distressed enough to seek care but not be of a severity requiring (traditional) face-to-face treatment.
As shown in Figure 1: During the period depicted, SilverCloud experienced growth, while utilization of the Employee Assistance Program (and referrals to behavioral health) declined.
Figure 1: SilverCloud and EAP Utilization
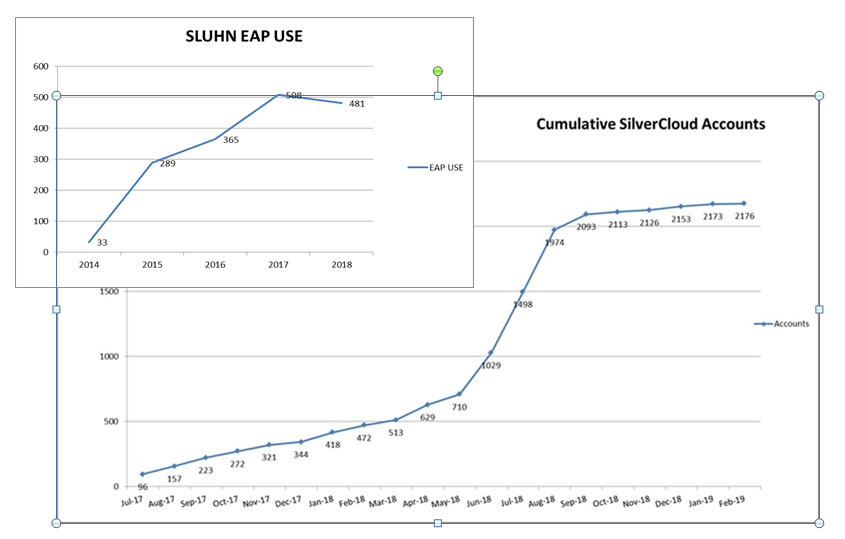
Source: St. Luke’s University Health Network
Providing an easily accessible, stigma-free and confidential mental/behavioral health platform seems to have confirmed our baseline data of existing need by exceeding our utilization goals while also diverting, at least to some degree, the destination of those who previously would have had no choice but to use the EAP.
Improving Patient Outcomes
St. Luke’s partnership with SilverCloud was successful in providing accessible mental/behavioral health options to the employee population and their spouses. Outcomes were captured in a variety of ways as illustrated on the series of Figures listed below.
Employees who engaged with SilverCloud programs saw measurable improvement in symptoms related to depression and anxiety. Figure 2: highlights the Space from Depression Program. Out of 1,042 responders to the PHQ-9:
- 71% of participants with moderately severe depression and 50% of those with severe depression reported clinically significant improvement (3+ reduction to PHQ-9 score) of symptoms by the end of the program.
Figure 2: Space from Depression – Improvement and Clinically Significant Improvement by Baseline Severity
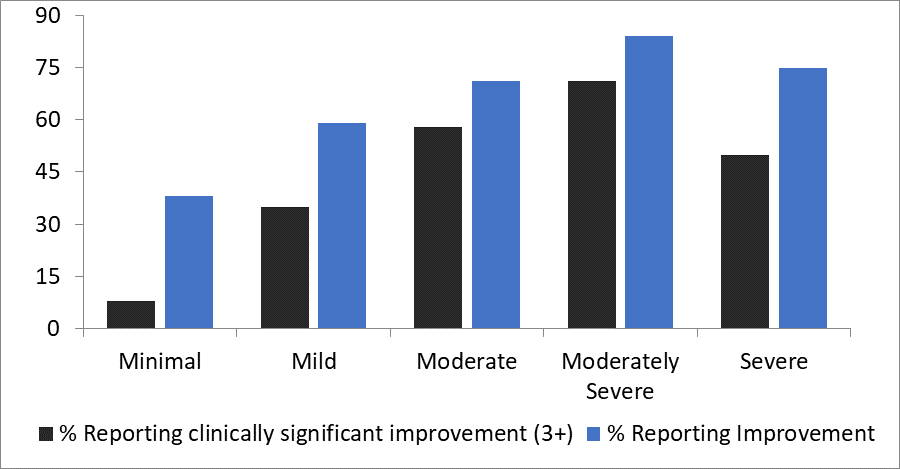
Source: St. Luke’s University Health Network
Figure 3: highlights the Space from Anxiety Program. Out of 1,038 responders to the GAD-7:
- 52% of participants with moderate anxiety and 62% of those with severe anxiety reported clinically significant improvement (3+ reduction to GAD-7 score) after using SilverCloud.
Figure 3: Space from Anxiety – Improvement and Clinically Significant Improvement by Baseline Severity
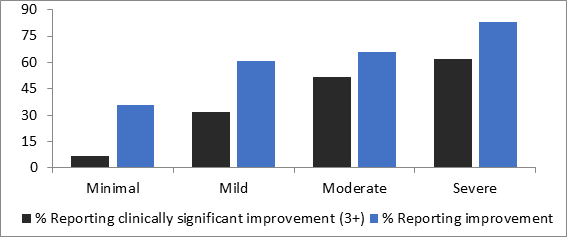
Source: St. Luke’s University Health Network
Nearly 33% of employees who exhibited moderate symptoms of depression or anxiety at baseline experienced a clinical remission of symptoms. Meaning their PHQ-9 or GAD-7 assessment scores dropped to a five or below after completing the platform. Figures 4 and 5 further look at this breakdown by examining the PHQ-9 and GAD-7 scoring of participants who completed their respective programs.
Figure 4: Compares the changes in symptom severity of 913 completed participants depression, as measured by initial/baseline and exiting PHQ-9 scoring.
- 28 individuals (or 3% of participants) entered the platform with severe symptoms; with 22 individuals (or 2% of participants) exiting the platform with severe symptoms. Resulting in a 1% reduction in severe symptoms, for the SilverCloud Platform, upon completion.
- 61 (or 7%) entered the platform with moderately severe symptoms; with 34 (or 4%) exiting. Resulting in a 3% reduction in moderately severe symptoms upon completion.
- 137 (or 15%) entered the platform with moderate symptoms; with 93 (or 10%) exiting. Resulting in a 5% reduction in moderate symptoms upon completion.
- 248 (or 27%) entered the platform with mild symptoms; with 222 (or 24%) exiting. Resulting in a 3% reduction in mild symptoms upon completion.
- 439 (or 48%) entered the platform with minimal symptoms; with 542 (or 59%) exiting. Resulting in a gain of 11% (or 103 individuals) having meaningfully reduced the severity of their depression symptoms.
Figure 4: PHQ-9 Scoring, Pre- and Post-SilverCloud Program Completion
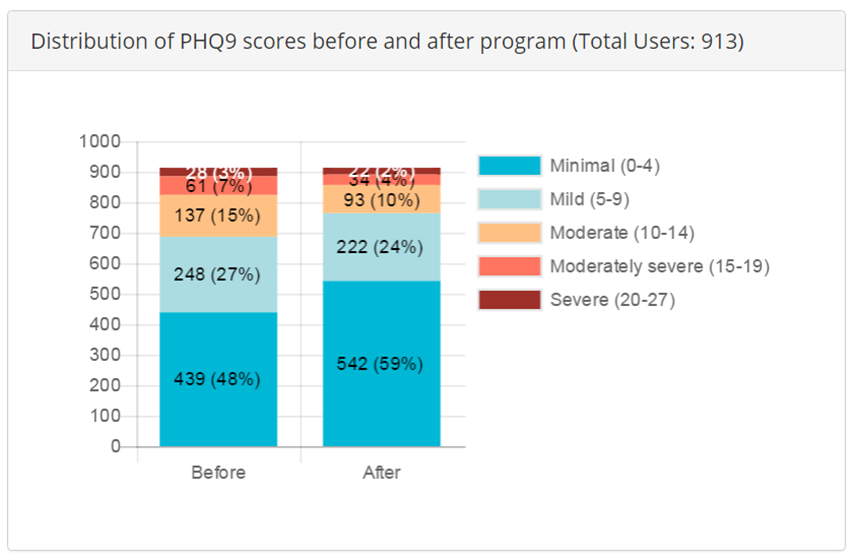
Source: St. Luke’s University Health Network
Figure 5: Compares the changes in symptom severity of 907 completed participants generalized anxiety, as measured by initial/baseline and exiting GAD-7 scoring.
- 107 individuals (or 12% of participants) entered the platform with severe symptoms; with 68 individuals (or 7% of participants) exiting the platform with severe symptoms. Resulting in a 5% reduction in severe symptoms, for the SilverCloud Platform, upon completion.
- 133 (or 15%) entered the platform with moderate symptoms; with 98 (or 11%) exiting. Resulting in a 4% reduction in moderate symptoms upon completion.
- 259 (or 29%) entered the platform with mild symptoms; with 229 (or 25%) exiting. Resulting in a 4% reduction in mild symptoms upon completion.
- 408 (or 45%) entered the platform with minimal symptoms; with 512 (or 56%) exiting. Resulting in a gain of 11% (or 104 individuals) having meaningfully reduced the severity of their generalized anxiety symptoms.
Figure 5: GAD-7 Scoring, Pre and Post SilverCloud Program Completion
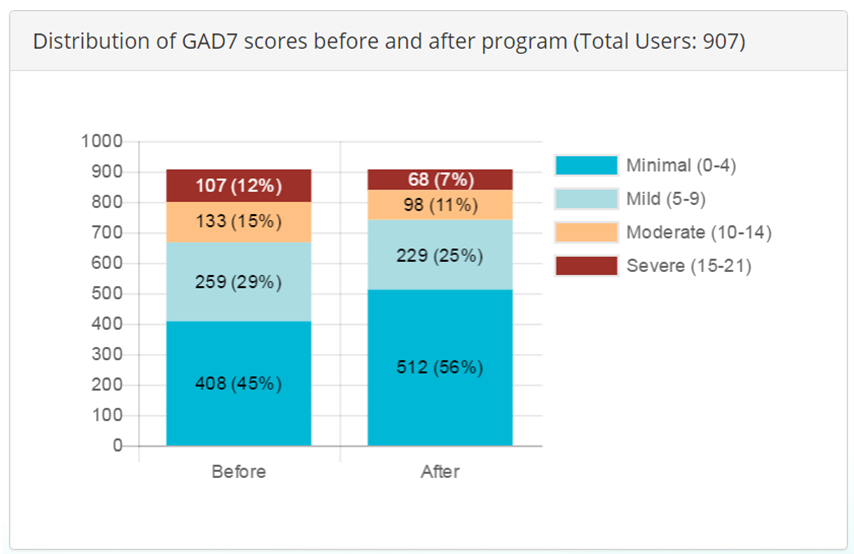
Source: St. Luke’s University Health Network
Due to the participant anonymity, we are unable to determine individual shifts in severity, so it becomes impossible to say what number of participants experienced an increase or reduction in acuity, but we can see the SilverCloud Platform’s overall performance when examining the baseline and exit PHQ-9 & GAD-7 scores of completed participants. As shown, overall severity is reduced.
Accountability and Driving Resilient Care Redesign
The value of any innovation must be weighed against its sustainability. Lowering costs is important, but less so, if the service is unused. Likewise, quality is important, but not at the expense of incurring additional costs. The holy grail would be a sustainable service line that is not only cheaper than existing options, but also has customer appeal. The SilverCloud platform does both things.
Participants who completed the program felt there was value in the experience. They were asked periodically throughout their engagement to comment on the program’s material, content, presentation and design, among a variety of other things. The results as shown below in Figure 6, were overwhelmingly positive.
Figure 6: User Satisfaction
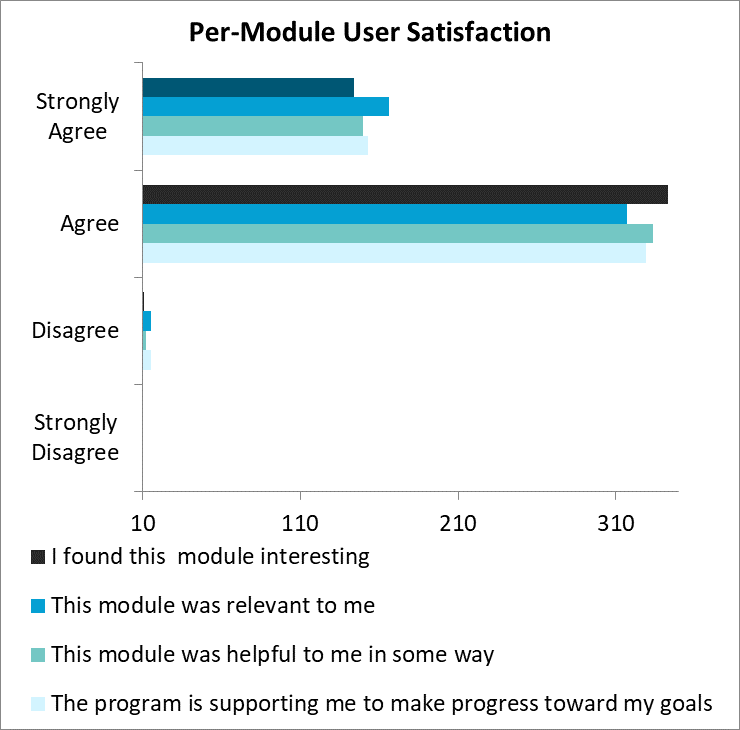
Source: St. Luke’s University Health Network
St. Luke’s partnership with SilverCloud Health helped drive better mental health outcomes for employees, which in turn allowed the organization to realize significant cost savings.
For those employees who met the clinical threshold for anxiety and depression, it’s estimated that St. Luke’s saved $17 for every $1 spent on SilverCloud.
Figure 7: Financial Savings of SilverCloud Treatment vs Face to Face Treatment for Users with Caseness*
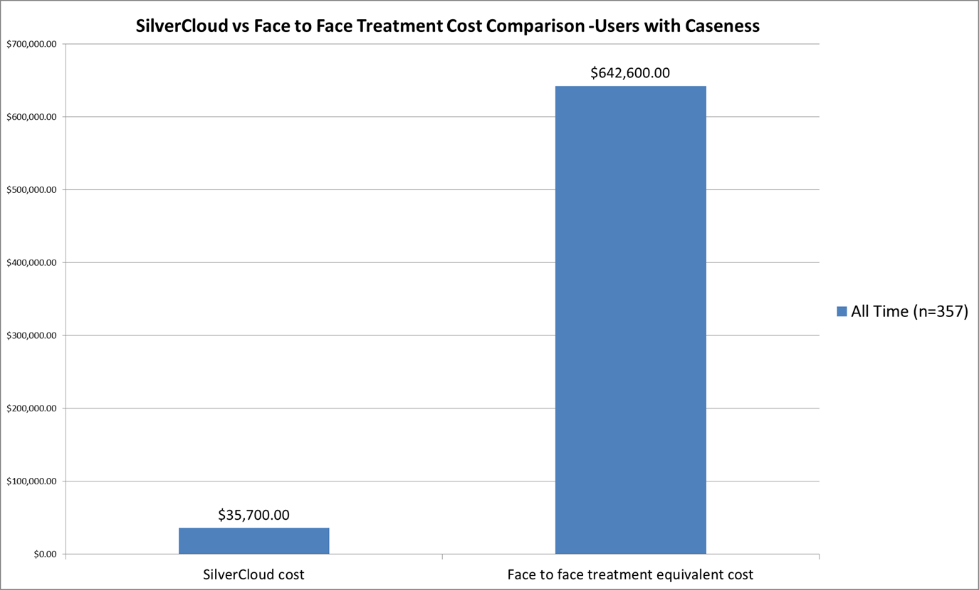
Source: St. Luke’s University Health Network
*Caseness indicates user meets clinical threshold for diagnosis at account creation (n=357)
Figure 8: Financial Savings of SilverCloud Treatment vs Face-to-Face Treatment for Users with Caseness and Reliable Recovery
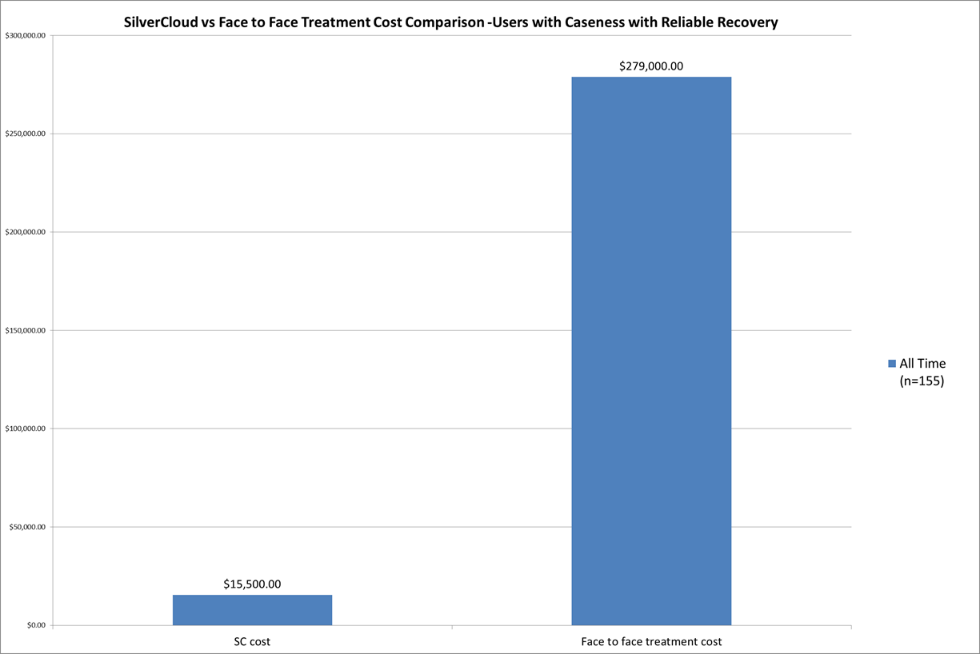
Source: St. Luke’s University Health Network
*Reliable recovery indicates users had a reliable reduction (4 points for PHQ-9 or 6 points for GAD-7) and fell below the clinical threshold (n=155)
Notably, the SLUHN implementation of SilverCloud was the first that involved a full-time employee to support the platform. It was also unique in that SLUHN was the first company to implement the program to an employee population. The results of this have been exceptional and serve as a benchmark for other organizations rolling out their own services.
Moving forward, SilverCloud continues to be available to SLUHN employees and spouses. It has proven, from the beginning, to be a viable, accessible and strategic asset in providing employees and their spouses with much needed mental/behavioral health resources while also serving as an intermediary for the supply/demand mismatch between patients/clients and traditional services. The SilverCloud Platform is both referred to, as well as regularly referring to, both internal and community facing resources.
Additional content is regularly added to the platform. New programs and tweaks to existing content are an ongoing collaboration between the developer and our existing in-house subject matter experts. St. Luke’s meet regularly with the vendor to discuss portal improvements based on user experience and supporter feedback, as well as review new modules for suitability to our populations to increase our content library.
During the COVID-19 pandemic, SilverCloud was an early adopter for content meant to ease the stress of these challenging times. Since the platform is accessible online, many individuals continued to access their accounts, while others discovered for the first time the access they have to this much needed resource.
SilverCloud has been well received and continues to score high marks in user satisfaction while meeting targeted participation goals and demonstrating positive outcomes in caseness, recovery, reliable change and reliably recovered metrics.
In short, the pilot was a success. The adoption, utilization and outcomes exceeded the expectations of the Employee Wellness Team, SilverCloud Planning Team and the SilverCloud creators.
But where do we go from here?
Due to our employee implementation being anonymous, we are limited in ability to analyze identified outcomes and claims data. SLUHN is working to expand the availability of SilverCloud to two pilot patient populations, aiming to replicate the clinical and cost savings success of the employee program. In these new pilot scenarios, demographic data will be collected to facilitate further data analysis. The vendor has also let us know that they are working with EPIC to build an integration between SilverCloud and the EMR, which may facilitate future use and data analysis.
Other healthcare provider organizations considering using similar technology should begin by deciding on what level of intervention/treatment the organization wants to provide. Self-guided vs. supported technologies differ in their targeted audiences and thus expected effectiveness/outcomes. For example, a meditation app may be proven to have statistically significant results in lowering stress levels, but that is quite different then a supported app based on cognitive behavioral therapy, meant to help reduce the acuity of symptoms for depression and anxiety. They should do their own research and pick a platform/tool that is proven clinically effective while being able to meet the organization’s expectations. For example, we decided to ensure the anonymity and confidentiality of participants, which likely increased engagement, but directly limited the ability to measure certain downstream effects caused by the utilization of services.
An ongoing marketing plan was also key to the success of the project.
Figure 9: SilverCloud Marketing Timeline
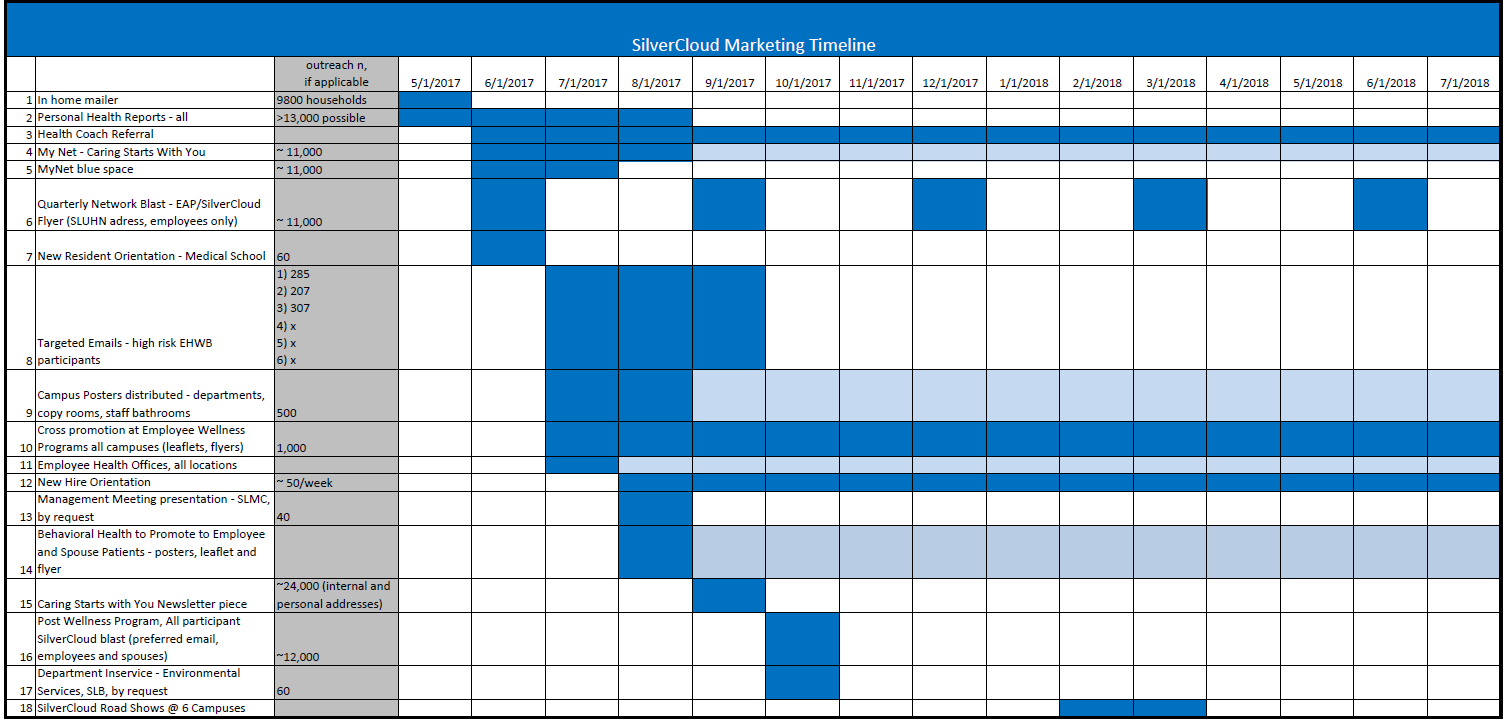
Source: St. Luke’s University Health Network
The views and opinions expressed in this content or by commenters are those of the author and do not necessarily reflect the official policy or position of HIMSS or its affiliates.
HIMSS Davies Awards
The HIMSS Davies Award recognizes the thoughtful application of health information and technology to substantially improve clinical care delivery, patient outcomes and population health.



